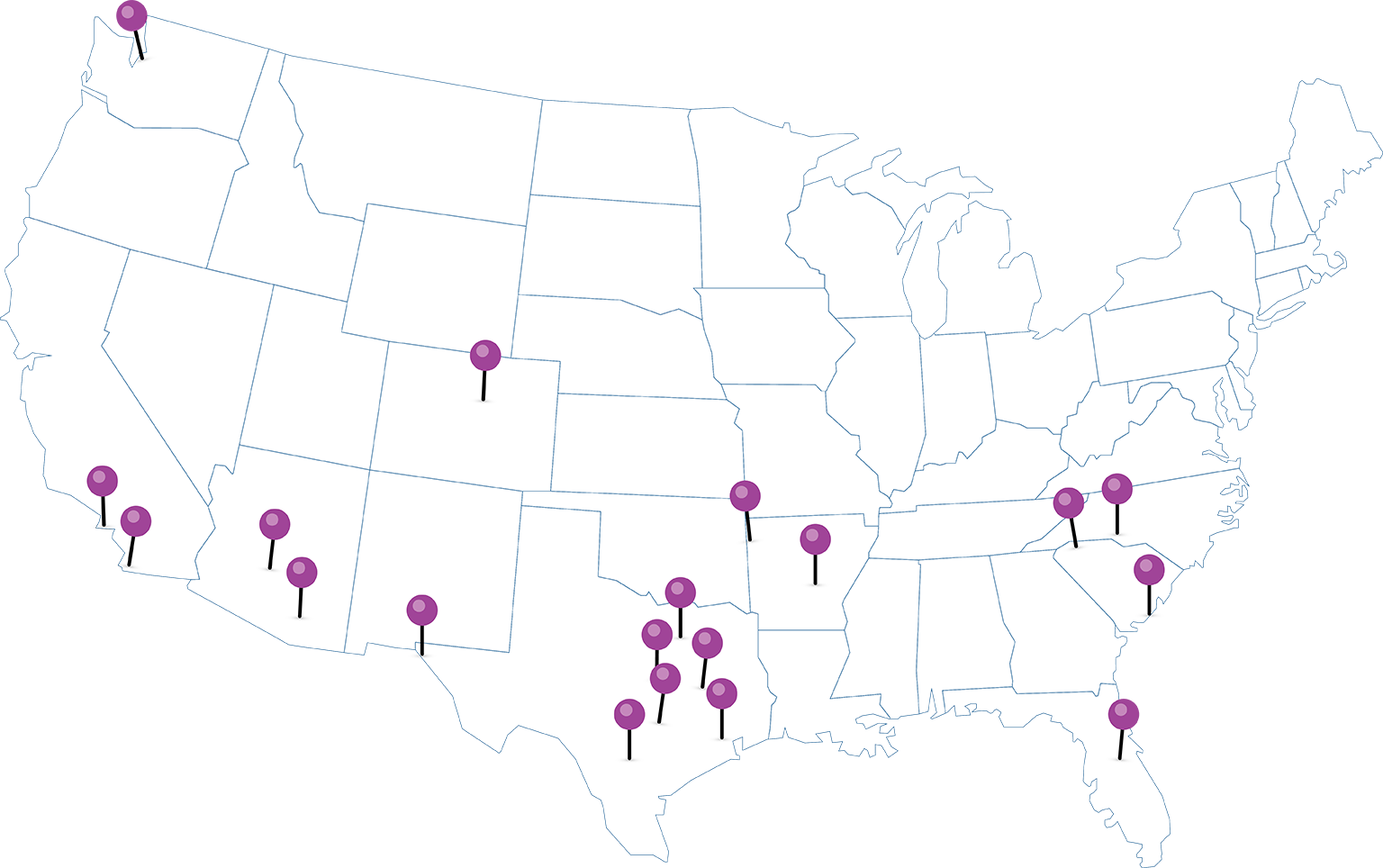
Where Can You Find Us?
EHN Regions
Austin, TX
Charleston, SC
Charlotte, NC
College Station, TX
Dallas & Fort Worth, TX
Denver, CO
El Paso, TX
Fort Smith, AR
Greenville & Spartanburg, SC
Houston, TX
Little Rock, AR
Los Angeles, CA
Orlando, FL
Phoenix & Tucson, AZ
San Antonio, TX
San Diego, CA
Seattle, WA
Temple, TX
EHN by the Numbers

Surveyed members gave EHN a 4.7 out of 5 rating for member engagement over the past 3 years.
EHN has partnerships with 20 leading health system partners across 18 regions (and growing).

EHN members have access to 9,000+ facilities and 85,000+ practitioners (and counting).
EHN provides savings of greater than 20% against traditional PPO network models.
What are EHN clients and partners saying?
EHN helps bridge the gap between employers and providers so we can do what we do best: deliver high quality service, local access, convenient navigation and care management that helps control rising costs,” said Brian Felty, vice president business development, Baylor Scott & White Health. “We work together to remove administrative burdens and improve the overall healthcare experience in the Dallas-Fort Worth market.
BSWQA
EHN gives me the best of both worlds, relationships and results. Managing a high performance health plan is still not easy and never will be, but the team at EHN is always responsive, always has a solution, and always plays well on the team we assemble to help a specific employer. They do what they say they are going to do and never let us down when they tell us they will follow up. Although a follow up is rarely needed, as there always seems to be a friendly voice willing and able to help on things we call in for when an escalation is needed. EHN has not been a vendor or a network for us, they’ve been a true partner to our agency and the employer groups we serve.
- Broker Partner
We are constantly looking for innovative solutions for our employer clients, and we have found such with Employer’s Health Network . EHN has been a partner that delivers on their promises, and that aligns with our values as an organization. I am proud to endorse EHN for living out those values in what they do.
-Broker Partner